There’s been a lot of news coverage about measles recently, including a growing outbreak in western Texas. Why are we seeing rising case counts and outbreaks, and does it mean an outbreak is more likely where you live?
Back to basics – let’s start with an overview of measles:
Clinical Presentation and Complications
Measles is known for its characteristic full body rash, starting at the hairline and moving downward along the body, and the ‘3 C’s’: “Cough”, “Coryza” (runny nose), and “Conjunctivitis” (red, watery, irritated eyes). Measles can also cause a very high fever, and ~20% of measles patients are hospitalized. Up to 1 in 20 patients may develop pneumonia, and 1-3 per 1,000 patients will die. In short, measles is not a mild illness.
Through deployments, I have actually seen measles patients up close, and their illness is not something I would want to risk for myself, my friends, or my family. In addition to the previously mentioned risks, patients can rarely (7-11/100,000 patients) develop subacute sclerosing panencephalitis (SSPE), a progressive neurological complication that strikes up to 10 years after acute measles infections, and invariably leads to death. Recent research has also identified that measles infection can cause ‘immune amnesia’ – where measles patients face immune suppression for a few years after acute infection.
Transmission
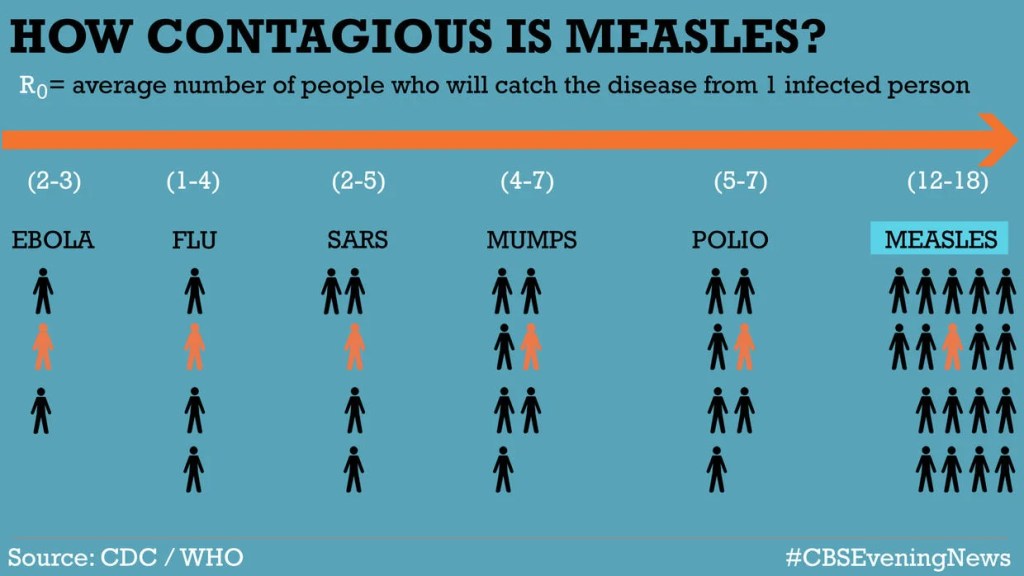
Measles is a respiratory virus that can spread through airborne transmission. Measles has the distinct honor of being the most contagious human virus. The R0, or the basic reproduction number, of a pathogen describes how many people are infected, on average, by one infectious case in a fully susceptible population. The R0 for the flu is between 1-4. For measles, the R0 is between 12 and 18 – meaning that each case of measles, on average, infects over a dozen additional individuals in a fully susceptible population.
You can imagine how fast measles outbreaks can spread in unvaccinated populations. Measles virus can also stay suspended in the air and remain contagious for up to 2 hours after an infectious person leaves a room, meaning that someone could get measles just from walking into a space where a patient with measles was hours before.
Epidemiology of Measles in the US
Since the measles vaccine was introduced in 1963, there has been a >99% decrease in measles cases. The vaccine is so successful that measles, once a universal childhood illness, was declared ‘eliminated’ from the Americas in 2000. This elimination designation meant that measles was no longer circulating in the US.
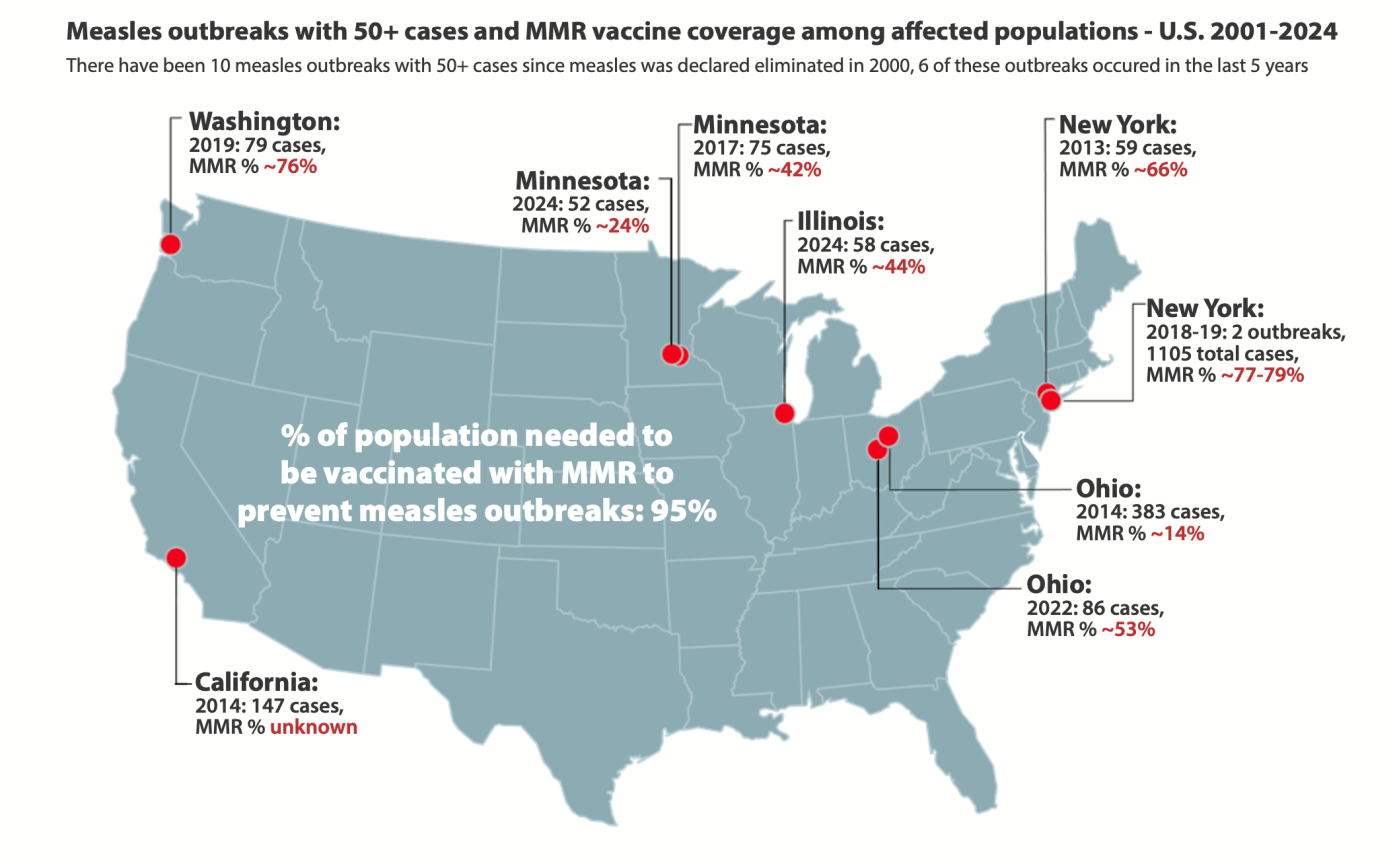
I spent most of my PhD working on the mathematical implications of clustering of non-vaccination on herd immunity, specifically for measles. Herd immunity is the concept that if you reach a critical immunization level in a population, you can stop transmission. This threshold is determined by the R0 of the pathogen – the higher the R0, the higher the herd immunity threshold. For measles, the herd immunity threshold is 95%. In the US, the overall MMR vaccination coverage is 92.7%, which is close, but not at, the threshold.
However, when non-vaccinators are socially or spatially clustered, outbreaks can occur even if the herd immunity threshold is met at the county, state, or national level. People do tend to cluster with others who have similar behaviors and beliefs, and these clusters, or close-knit, unvaccinated communities, are most at risk for large and disruptive measles outbreak.
We can look at this map of all the large measles outbreaks in the US since elimination from CDC. Outbreaks with 50+ cases are considered ‘large’. There were 10 outbreaks with 50+ cases from 2001-2024. These outbreaks occurred in areas with MMR vaccination coverage far below the 95% level, and all but two occurred in close-knit, undervaccinated communities.

So, what’s going on in Texas?
The measles outbreak in Texas has grown to 90 cases in just 4 weeks, indicating the potential for explosive growth. Looking back at the map of large outbreaks since elimination, only four outbreaks since elimination have exceeded 90 cases: the Disneyland outbreak in 2014, two NY outbreaks among the Haredi population in 2019, and an outbreak in Ohio in 2014 among an Amish population. The Texas outbreak has a lot of room to grow, it’s just getting started.
This outbreak is worrisome for a few reasons:
- There has been rapid growth in just 1-2 incubation periods, meaning there are a lot of people who currently have measles in Gaines County Texas (57 infections in Gaines County alone), 20 cases in Terry county, and a handful of cases in neighboring counties.
- Tuesday’s update had 58 cases, meaning there was an increase of 32 cases in just three days. This suggests the force of infection in this outbreak is extremely high. This rapid growth is fairly unprecedented for recent measles outbreaks in the US.
- Gaines County has one of the highest rates of vaccine exemptions in Texas – the Seminole school district had a ~14% exemption rate in the 2023-2024 school year, with MMR coverage only 81.97%.
- This outbreak is occurring in a close-knit, undervaccinated community – specifically a Mennonite community. Many of the families in this community attend religious schools or are homeschooled, and vaccination rates are very low. These outbreaks can continue for a long time without strong public health measures.
- There are cases across the border in New Mexico – nine so far. There has been no identified link between the outbreak in Texas and this outbreak, known as an ‘epidemiological link, or epi-link’. That could suggest community transmission in this geography.
- This part of the country hasn’t had a measles outbreak in a long time – this outbreak is Texas’ worst in 30 years. While the state and local health departments have lots of outbreak experience, they likely don’t have a lot of recent measles experience. Large measles outbreaks require lots of coordination between local, state, and federal public health, and can be extremely expensive.
What does this mean for you?
Most Americans aren’t at increased risk of measles as a result of this outbreak – but if you live in the South Plains Public Health District, you are at higher risk of exposure to measles. If you live in that region, now is the time to check your vaccination status. You can best protect yourself by being up to date on the MMR vaccine (2 doses, the first at 12-15 months, and the second at 4-6 years), which will give you 97% protection.
However, some factors have increased measles risk for all Americans:
- Global measles incidence has been on the rise: in 2019, the US almost lost elimination status due to large outbreaks in New York. The COVID-19 pandemic ushered in a period of relative calm and suppressed transmission of many infectious diseases, measles included, but measles came roaring back in 2024, with 285 cases and 16 outbreaks.
- We are living in a period of anti-vaccine backlash. Some states have taken extraordinary measures to buck historical precedent and stop treating measles with the tools needed to control outbreaks: case investigation, isolation of cases, quarantine of susceptible contacts (including school exclusion), and mass vaccination.
- COVID-19 changed the way many of us think about vaccines, and there is evidence that vaccine hesitancy increased across the board as a result of the pandemic.
- In 2024 – Florida made the news for not excluding unvaccinated, exposed children from school during a measles outbreak
- Just last week, Louisiana said it would stop promoting mass vaccination
- RFK Jr. is the new HHS Secretary, a man who himself has spread anti-vaccine beliefs, and fueled anti-vaccine sentiment in close-knit communities, contributing to a deadly outbreak of measles in Samoa
All of these changes signal high-level normalization of anti-vaccine beliefs, which increases the risk for Americans. Larger measles outbreaks typically end in one of two ways:
- Outcome #1: Public health officials respond quickly and effectively, instituting case finding, case isolation, quarantine/exclusion of susceptible contacts, and mass vaccination campaigns in areas experiencing outbreaks.
- Outcome #2: Measles infects nearly all susceptible individuals in a community, slowing down only when the pool of people to infect is depleted.
Outcome #2 is especially concerning in close-knit undervaccinated communities, where there are a lot of susceptible people. If state and local health departments don’t utilize (or aren’t able to) the tried and true public health tools needed to bring a measles outbreak under control, the outbreak could grow to many hundreds of cases. If case counts grow enough, there is risk of spillover from the Mennonite community to the general community in Texas/New Mexico, which would put many more Americans at risk of contracting measles.
The anti-vaccine climate we’re living in makes measles outbreaks more likely everywhere, but particularly in or near close-knit, unvaccinated communities. With more frequent outbreaks, it’s prudent to check your and your children’s MMR records and ensure everyone is up to date. While we can’t fully control our environment, we can control our own immunization status.
Wonderful summary of measles epidemiology and the issues we are facing to control measles. David Wood, MD, Pediatrician
LikeLike